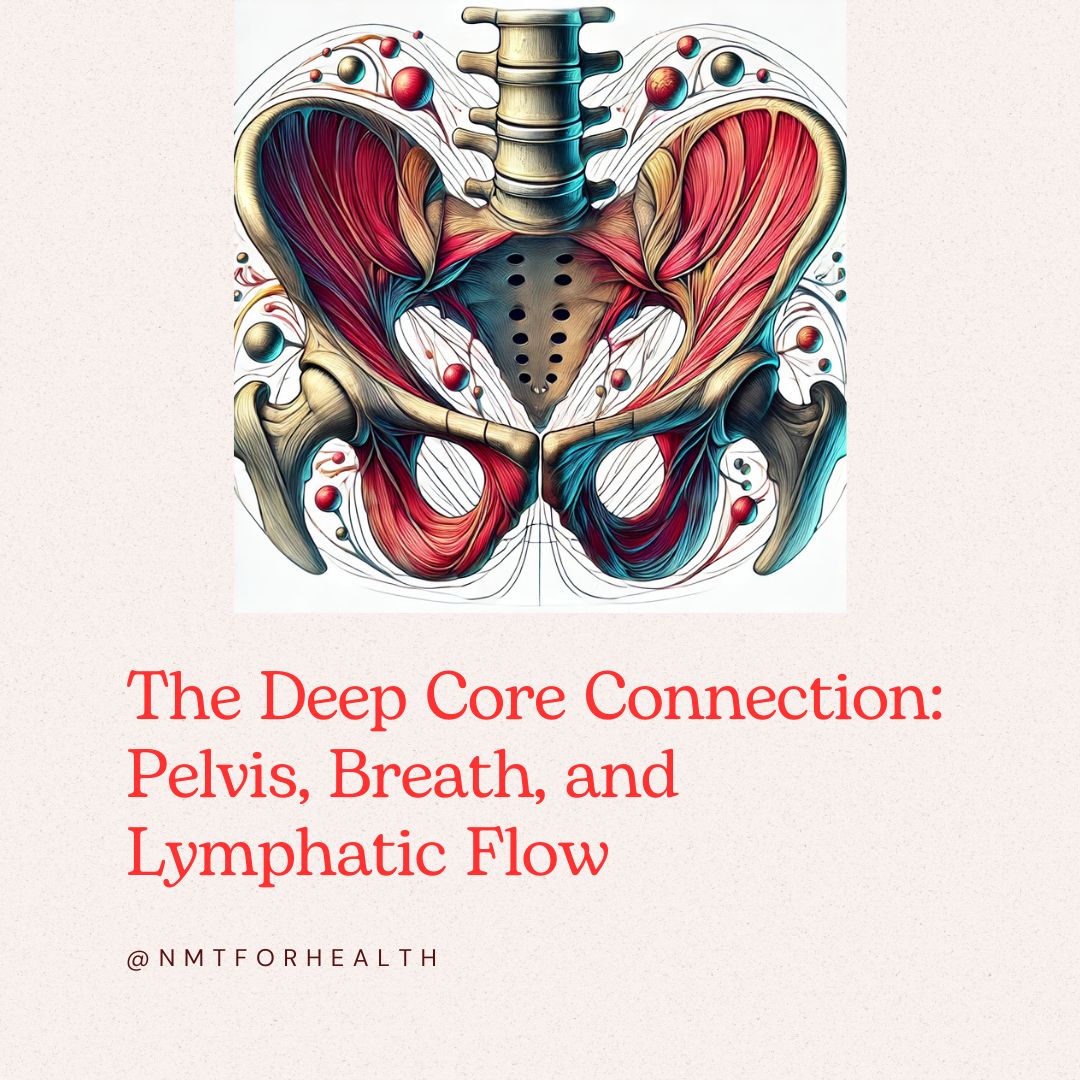
When it comes to bone health, skeletal adaptation, and movement efficiency, the pelvis and its deep core muscles play a far greater role than most people realize. While conversations about osteopenia, osteoporosis, and skeletal resilience tend to focus on the spine, hips, and wrists, we rarely consider how underutilized intrinsic muscles influence overall bone health—until dysfunction forces us to.
In Part 1 of the Natural Stack Series, we explored how breathing powers core stability. In Part 2, we uncovered how quad dominance disrupts movement and balance. Now, we turn to the pelvis and deep core, the foundation for how the body absorbs impact, stabilizes joints, and distributes tension—factors that directly affect skeletal integrity and long-term bone health.
This post will cover:
- The anatomy and function of the deep core system
- Why these muscles are often underutilized
- The impact of core weakness on bone adaptation and skeletal health
- The pelvis-jaw connection and its role in stress, tension, and movement compensation
The Overlooked Muscles That Support Bone Health
Bone health isn’t just about density—it’s about how forces are absorbed, distributed, and transferred through the body. The intrinsic deep core muscles form the foundation of this system, working with the pelvis, spine, and breath to create stability without rigidity.
Anatomy of the Deep Core System
At the deepest level of movement control, we find:
1. The Pelvic Floor
A network of muscles that:
- Supports the spine, hips, and abdominal organs
- Balances intra-abdominal pressure
- Coordinates with breathing and postural control
2. The Transverse Abdominis (TVA)
The deepest layer of abdominal muscles, wrapping around the midsection like a corset to provide:
- Core stabilization without bracing
- Support for spinal alignment
- A direct connection to breath and pelvic movement
3. The Multifidus
A deep spinal stabilizer that:
- Provides segmental spinal control
- Supports skeletal alignment under load
- Works reflexively with the pelvic floor
4. The Diaphragm
A key part of the core stabilization system, influencing:
- Breath-controlled core activation
- Regulation of intra-abdominal pressure
- The connection between posture, stability, and movement patterns
These muscles work together to protect bones, prevent excessive strain, and maintain skeletal balance. When they’re weak, inactive, or poorly coordinated, the body compensates—leading to excessive force on bones, altered movement patterns, and increased tension elsewhere.
Why These Muscles Are Underutilized
Despite their importance, many people fail to engage their deep core properly. Here’s why:
1. Poor Breath Mechanics
Shallow breathing disconnects the diaphragm from the core system, weakening pelvic stability and making it harder for the spine and pelvis to absorb force efficiently.
2. Over-Reliance on Larger Muscles
When intrinsic stability is weak, the body compensates by bracing with superficial muscles—like the quads, glutes, and external obliques—leading to rigid movement and excessive tension instead of fluid stability.
3. Pelvic Misalignment & Bone Health
A misaligned pelvis doesn’t just affect movement—it changes how bones experience force, influencing how bone remodeling occurs over time.
Studies show that asymmetrical movement and poor postural control increase mechanical stress on bones, which may contribute to bone loss in underloaded areas (National Library of Medicine).
This is especially relevant in osteopenia and osteoporosis, where bones lose their ability to adapt to mechanical loading efficiently—a process exacerbated by unbalanced muscle engagement.
This brings us to a key connection: how skeletal adaptation in the pelvis and jaw affects deep core function—and why ignoring this relationship can lead to unnecessary tension and inefficient movement patterns.
The Jaw-Pelvis Connection & Skeletal Adaptation
Studies on perimenopause and menopause-related bone changes suggest that jawbone structure may change alongside other skeletal adaptations, similar to shifts seen in bone remodeling and muscle function over time (National Library of Medicine).
Perimenopause is a time when movement strategies can support skeletal health, as hormonal shifts influence muscle activation, postural balance, and how the body distributes tension.
While jaw tension doesn’t necessarily indicate an underlying bone issue, persistent clenching or TMJ discomfort can sometimes be linked to:
- Movement patterns
- Muscle compensation
- Postural habits
When pelvic stability is compromised, the body compensates by gripping elsewhere—most commonly in the jaw, neck, and shoulders. Over time, this leads to:
- Increased nervous system tension – The body stays in a low-level stress response, reinforcing chronic clenching patterns.
- Reduced skeletal adaptability – Bones adapt to force patterns, so tension-based stability may limit natural bone remodeling.
- Breathing dysfunction – Shallow breathing disrupts deep core activation, further weakening pelvic control.
Ignoring this pelvis-jaw connection can create chronic tension patterns that affect movement, breath efficiency, and bone resilience.
How to Restore Deep Core Function for Bone Health
1. Reconnect Breath & Core Stability
Try this – 5 minutes
Since the pelvic floor, diaphragm, and deep core muscles must work together, restoring breath control is key.
Try this:
- Sit or lie down comfortably.
- Inhale through your nose, feeling your ribs expand outward.
- Exhale fully through your mouth, allowing your pelvic floor to gently lift.
- Repeat for 5 minutes, noticing how breath connects to deep core activation.
2. Release Jaw & Pelvic Tension Together
Try this – 3 minutes
Since jaw and pelvic tension are linked, relaxing one can help the other release.
Try this:
- Gently place your tongue on the roof of your mouth.
- Slowly exhale, allowing your jaw to relax.
- Notice if your pelvic floor subtly releases at the same time.
- Repeat for 3 minutes before movement practice.
3. Train Functional Core Stability
Try this – 7 minutes
Focus on movements that integrate deep stabilization rather than traditional bracing exercises.
Try this:
- Single-leg stance (2 minutes) – Improves pelvic and deep core control.
- Dead bug variations (3 minutes) – Engages TVA and trains reflexive core activation.
- Pelvic tilts with breath (2 minutes) – Helps retrain pelvic stability and diaphragm function.
Key Takeaways
- 🦴 Deep core muscles—including the pelvic floor, transverse abdominis, multifidus, and diaphragm—are essential for skeletal health, stability, and movement efficiency.
- 💨 Poor breathing mechanics and underutilized core muscles can lead to compensation patterns, affecting posture, bone adaptation, and overall function.
- 🔄 The jaw-pelvis connection highlights how tension in one area (like the jaw) can reflect imbalances elsewhere, impacting the body’s ability to stabilize and adapt.
- 🏋️♀️ Simple strategies—like breathwork, functional core exercises, and tension release—can help restore deep core engagement, support bone health, and improve movement patterns.
Building the Natural Stack: Why This Matters
In the Natural Stack Series, we’re uncovering how every layer of movement is interconnected. Breath (Part 1), quad dominance (Part 2), and deep core activation (Part 3) all contribute to full-body balance, function, and resilience.
When we restore deep core engagement, we:
- Reduce compensation patterns that create chronic tension
- Improve balance and skeletal alignment
- Support the nervous system and breath function
- Strengthen foundational movement for longevity
By reconnecting with your pelvis, breath, and jaw, you can build a foundation that supports lifelong movement and resilience.
References:
-
Critical Role of Estrogens on Bone Homeostasis in Both Male and Female
This study highlights the significant impact of estrogen on bone turnover and density in both sexes, emphasizing changes during menopause.
Link -
The Effect of General Bone Mineral Density on the Quantity and Quality of the Edentulous Mandible
Research indicating that reduced bone mineral density negatively affects the quality and quantity of jawbone, particularly in postmenopausal women.
Link -
Oral Health and Menopause: A Comprehensive Review on Current Knowledge and Associated Dental Management
This review discusses how menopause-induced hormonal changes can lead to oral health issues, including jawbone density reduction.
Link -
Lymphatic Anatomy and Biomechanics
An in-depth look at how muscle movements, including those of the diaphragm and skeletal muscles, facilitate lymphatic flow and overall fluid balance.
Link -
Lymphatic Smooth Muscle: The Motor Unit of Lymph Drainage
This article explores the role of lymphatic smooth muscles in propelling lymph and how their activity is influenced by physical stimuli.
Link -
Exercise and Bone Health Across the Lifespan
A comprehensive review of how physical activity influences bone density and strength, underscoring the importance of muscle engagement in skeletal health.
Link
This article is for educational purposes only and is not intended as medical advice. Please consult a healthcare professional for personalized guidance.
By including these references, you provide a solid foundation for the information presented, allowing readers to delve deeper into the subject matter.
Comments
One response to “The Missing Link: Pelvis, Deep Core & Bone Health (Natural Stack Series, Part 3)”
[…] Related article: The Missing Link: Pelvis, Deep Core & Bone Health (Natural Stack Series, Part 3) […]