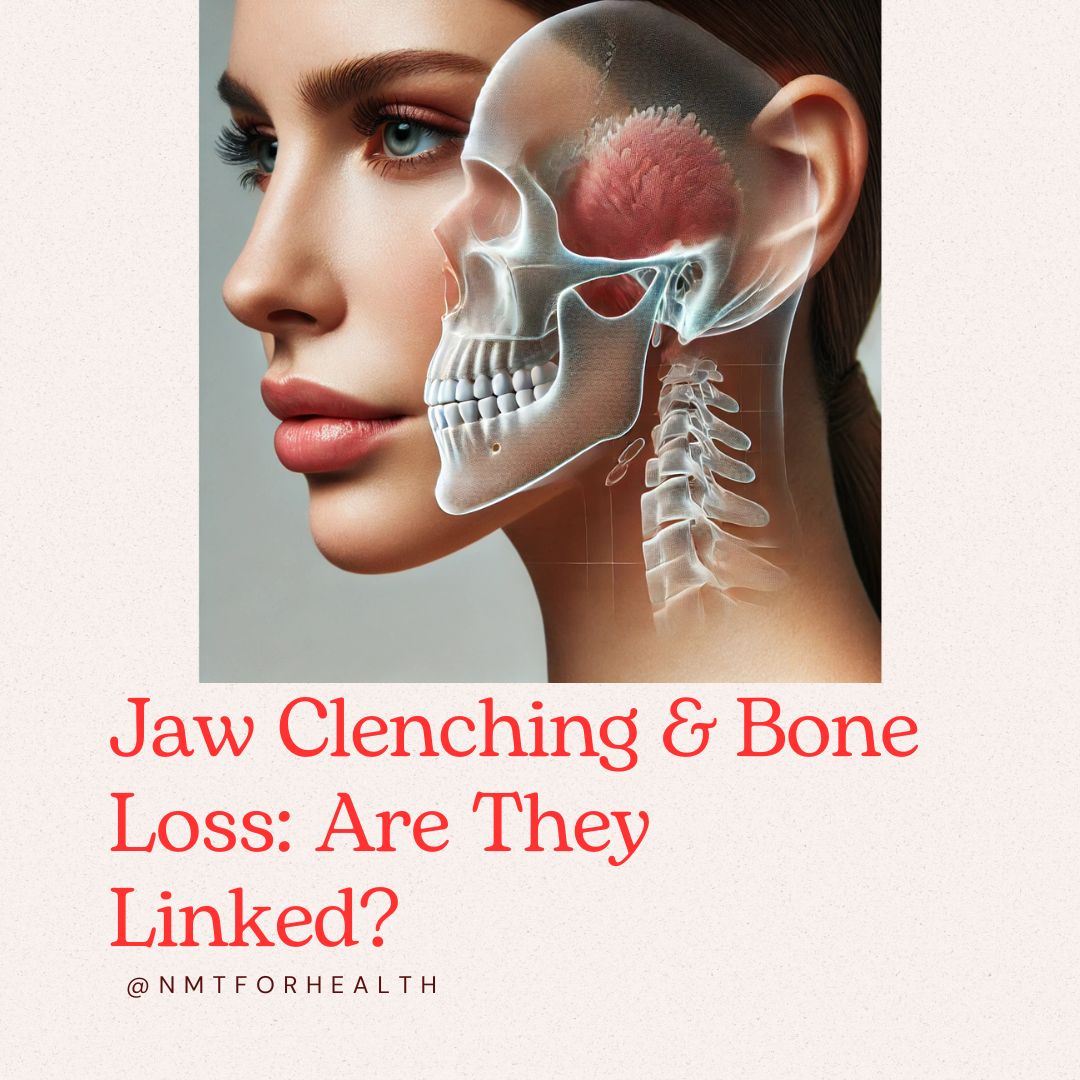
Ever noticed how your jaw feels tight after a stressful day? Most of us assume it’s just stress or teeth grinding, but what if it’s also reflecting something about how your body adapts over time?
Emerging research suggests that the jaw is more connected to overall musculoskeletal health than many people realize. While most discussions on bone density focus on the spine, hips, or wrists, studies indicate that jawbone changes can sometimes occur as part of broader skeletal adaptation. These shifts, particularly during perimenopause, menopause, and aging, can affect both women and men (National Library of Medicine).
What Your Jaw Might Be Telling You About Your Movement & Skeletal Health
Studies on perimenopause and menopause-related bone changes suggest that jawbone structure may change alongside other skeletal adaptations, similar to shifts seen in bone remodeling and muscle function over time (National Library of Medicine). Researchers propose that the jaw—like other bones in the body—responds to musculoskeletal adaptation throughout life.
Perimenopause is a time when movement strategies can support skeletal health, as hormonal shifts influence muscle activation, postural balance, and how the body distributes tension. Focusing on muscle engagement, movement quality, and postural awareness during this period may help optimize how the body adapts to change.
While jaw tension doesn’t necessarily indicate an underlying bone issue, persistent clenching or TMJ discomfort can sometimes be linked to movement patterns, muscle compensation, and postural habits. Some signs that your jaw may be reflecting broader musculoskeletal patterns include:
- More clenching and tension – The body may instinctively brace due to posture shifts or muscle imbalances.
- TMJ issues – Clicking, popping, or discomfort in the jaw may indicate muscular compensation.
- Changes in how your teeth fit together – Subtle shifts in bite alignment may be related to changes in jaw muscle activation.
- Persistent neck, shoulder, or facial tightness – These areas are closely linked through muscular and nervous system pathways.
That doesn’t mean jaw tension is a reason to panic—it’s something many people experience. But understanding these patterns can help you make small adjustments that support better movement, posture, and overall musculoskeletal balance.
Why Jaw Tension Affects More Than Just Your Mouth
Your Nervous System: Stuck in a Stress Loop?
The jaw is closely tied to the nervous system, which helps regulate tension and relaxation. Chronic jaw clenching has been linked to heightened autonomic nervous system activity, meaning that persistent tension can reinforce a prolonged fight-or-flight response (National Center for Complementary and Integrative Health).
Over time, this can contribute to:
- Difficulty fully relaxing
- Tension headaches and jaw discomfort
- Persistent tightness in the neck and shoulders
Training your nervous system to shift between tension and relaxation can help reset these patterns and prevent the cycle of chronic clenching.
Your Lymphatic System: Why Clenching Can Slow Recovery
Your lymphatic system plays a crucial role in removing waste, reducing inflammation, and supporting immune function. But here’s something often overlooked: muscle movement is essential for lymphatic circulation.
When muscles stay tense—especially in areas like the jaw, neck, and shoulders—lymphatic flow slows down, leading to:
- Swelling and puffiness (especially in the face and neck)
- Sluggish recovery after workouts or injuries
- A buildup of metabolic waste that can leave you feeling stiff and fatigued
Research suggests that lymphatic stagnation contributes to chronic inflammation, which can affect everything from muscle recovery to long-term mobility (Journal of Lymphatic Research and Biology).
If you’ve been dealing with persistent tightness, sluggish recovery, or inflammation, it might be worth looking at jaw tension and movement habits as part of the picture.
What You Can Do to Support Your Jaw, Movement, and Recovery
Start With Small Adjustments
Becoming more aware of your jaw tension doesn’t mean you need to overhaul everything. Small changes in how you breathe, move, and release tension can have a big impact over time.
1. Teach Your Nervous System to Relax on Command
Noticing tension is one thing—learning how to shift out of it is another. Somatic movement therapy and progressive muscle relaxation techniques can help train the nervous system to transition between activation and relaxation.
Try this: Before bed, lightly place your tongue on the roof of your mouth and let your jaw hang slightly open as you exhale. This small shift encourages relaxation in the jaw and nervous system.
2. Breathe the Right Way to Ease Jaw Tension
Breathing patterns directly affect muscle tension, including in the jaw. Shallow, chest-based breathing can reinforce tightness, while proper ribcage expansion helps support better muscle engagement and relaxation.
Try this: Place your hands on your ribs and inhale through your nose, directing the breath into the sides of your ribcage. Then, exhale fully through your mouth, allowing your jaw to soften at the end of the breath.
3. Strengthen Your Stability to Support Musculoskeletal Health
Movement plays a key role in skeletal and muscle adaptation. Stability exercises help train your body to transition smoothly between tension and relaxation while also supporting long-term posture and function.
Try this: Stand on one leg for 20 seconds, then switch sides. If this feels easy, try closing your eyes to challenge your balance.
4. Support Your Lymphatic System Through Movement
Since muscle movement is essential for lymphatic circulation, addressing jaw tension can help restore natural fluid flow, reduce puffiness, and improve tissue recovery.
Try this: Use gentle self-massage along your jawline, starting from your chin and moving toward your ears. This encourages lymphatic drainage and can help release built-up tension.
Want to Take This Work Deeper?
My book, Your Body’s Natural Stack, explores the deeper connections between movement, breathing, and long-term musculoskeletal health. It’s designed as a practical guide to the techniques I integrate into sessions, helping you support better posture, jaw function, and skeletal resilience.
By paying attention to how your jaw and body adapt over time, you can make small changes that support better movement, reduced tension, and overall well-being.
One Last Thing…
This article is for educational purposes only. If you have concerns about jaw pain, TMJ, or bone health, consult a healthcare provider for personalized guidance.
Related article: The Missing Link: Pelvis, Deep Core & Bone Health (Natural Stack Series, Part 3)
Comments
One response to “What Your Jaw Reveals About Your Bone Health”
[…] While jaw tension doesn’t necessarily indicate an underlying bone issue, persistent clenching or TMJ discomfort can sometimes be linked to: […]